It has been seven years since patient safety became recognised as a major international healthcare issue. Eisenberg’s analogy of patient safety having the characteristics of an epidemic of worldwide portions provides a framework of examining patient safety with three stages.
- Identify the risks and hazards that cause or have the potential to cause healthcare associated injury or harm
- Design, implement and evaluate patient safety practices that eliminate known hazards, reduce the risk of injury to patients and create a positive safety culture
- Maintain vigilance to ensure that a safe environment continues and patient safety cultures remain in place
For most of the past seven years patient safety movement has focused on stage one in the epidemic cycle with the primary action directed at the identification of risks and hazards to patient from healthcare associated injury or harm.
We are now just beginning to actively move to stage two of the cycle—the design and implementation but we are nowhere near reaching stage three. In examining new approaches to patient safety, it is important to review what we have learned in the past seven years at stage one to determine the directions for stage two.
Stage One: Identification of Risk and Hazards Retrospective and Prospective
Battles & Lilford noted that there are three primary sources of identifying risks and hazards that can be used for,
1) spontaneous active event reporting,
2) administrate data and
3) patient charts or records.
Significant progress has been made at implementing reporting systems at the institutional, regional and even the national level. There is growing recognition of the importance of using administrative or billing data in patient safety. The medical record continues to be a source of patient safety information but chart auditing is labour intensive. However newer approaches that use triggers with Electronic Health Records (EHR) are showing promise. When it comes to identifying risks and hazards retrospectively, we should apply a principle of maritime navigation which states that you can never truly know where you are without a three point fix of your position. Thus all three of these approaches are required to gain a complete picture of risks and hazards to patient safety.
Healthcare has relied almost exclusively on retrospective methods for risk assessment. This traditional epidemiologically based approach has been useful; however there is a growing need for more prospective or proactive approach to assessing risk and hazards in patient safety. Proactive risk assessment has been extensively used in a number of high hazard industries such as aerospace and nuclear power. The methods include Root Cause Analysis (RCA), process mapping, Failure Modes Effects Analysis (FMEA) and Probabilistic Risk Assessment (PRA). There is growing acceptance of the newer methods in patient safety and a call to combine both retrospective and prospective methods in order to gain a complete picture of the patient safety challenge.
Sensemaking
In order for organisations to become learning organisations, they must make sense of their environment and learn from safety events. Sensemaking, as described by Weick, literally means making sense of events. True sensemaking in patient safety must use both retrospective and prospective approach to learning. Sensemaking is an essential part of the design process leading to risk – informed design. The results of these separate or combined approaches are most effective when end users in conversation-based meetings add their expertise and knowledge to the data produced by, FMEA, and/or PRA in order to make sense of the risks and hazards. Without ownership engendered by such conversations, the possibility of effective action to eliminate or minimise them is greatly reduced.
Safety Culture Assessment
Safety culture assessment is an essential element at stage one of the epidemic cycle. Significant progress has been made in healthcare in measuring the culture of safety at the institutional and even the national level. The results: safety culture assessment can serve as a powerful starting point for organisations to implement patient safety projects in a positive atmosphere of improvement as well as measure progress of patient safety activities.
Stage Two – Safety by Design
The real challenge to patient safety is acting on the information obtained once the risk and hazards are identified. The design and implementation of interventions that are specially intended to eliminate or mitigate known risks and hazards is the challenge of stage two. Using the data collected in stage one, we need to move to a more risk—informed design approach to use proven design methods involving a number of professions outside of healthcare so that one could actually design out system failure and design in safety and quality of care.
Battles & Lilford have provided a modification of the Donabedian model to serve patient safety which uses a nested approach of structure surrounding process with human behavior at the core. This framework of structure and process can help determine what to design for the healthcare system. Figure 1 is a graphic representation of the nested model of the critical elements of structure and process that must be designed. This design model shares similar characteristics with Ferlie and Shortell model of the healthcare system and with Morey’s onion model of human factors design elements.
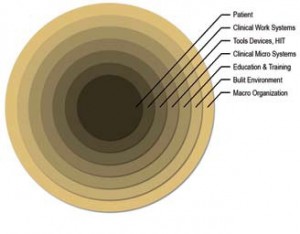
Figure 1
Clinical work is increasingly being supported and shaped by technology in the form of tools, devices and Health Information Technology (HIT). Technology represents a range of sophistication from automated laboratory testing and pharmaceutical dispensing equipment to robotic surgery devices to simple mistake-proofing devices.
The fact is that the tools of work are embedded into the process of care and are connected directly to the built environment. They must be designed in coordination with both the built environment and work itself. Automating broken work/clinical processes can and often do make matters worse rather than bring promised improvements.
The process of care can also be thought of as clinical work systems. Clinical work is an interaction of teams of healthcare providers working in micro systems within a built environment, using tools, devices and HIT to care for the object of the system i.e. the patient. The concept that work can be designed is not new. In healthcare, there has been a reluctance to shift away from the myth of the independent professional model of work to embrace the reality of interconnected clinical work systems. Clinical work can and should be designed for quality and safety.
Ineffective teamwork and communications continue to be listed as the main underlying cause of failure in patient safety events. This growing awareness of the importance of teamwork has led to the development of a number of successful programmes in teamwork training designed to improve the process of care. In addition to teamwork, the use of simulation as an implementation strategy that is showing great promise both as an intervention strategy and as a means to improve skills and performance across the continuum of care.
Conclusion
There is no simple quick fix or easy solution to the problems of patient safety. It requires hard work and commitment by everyone. There are a growing number of individual advances in patient safety that are and will continue to have an impact on the quality and safety of care. These advances must be looked at as a part of holistic or systems improvement rather than as a single solution to a very complex interconnected problem.
Unless there is a shared ownership of the risks and hazards associated with healthcare little progress will be made. This shared ownership of risk involves all levels of organisations from the Chief Executive Officers and the Board to all care givers and even to the janitors. It also includes government officials, those who pay for care and, of course, patients. When risks are known and fully understood, dealing with them is possible in a culture of safety.
About the Author
James B Battles, is a Senior Service Fellow for Patient Safety, Center for Quality Improvement and Patient Safety (CQuIPS), Agency for Healthcare Research and Quality (AHRQ, United States Department of Health & Human Services.






